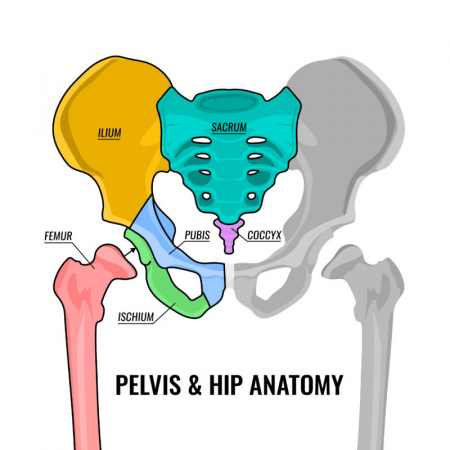
The pelvis is the lower part of the abdomen located between the hip bones. The basic structure is comprised of a bony ring and a number of supporting muscles, ligaments and tendons. It is an area which is richly innervated and which holds the reproductive organs, bladder, rectum and lumbosacral nerve plexus. The pelvis forms the base of the core and supports the weight of all the abdominal organs above it.
What is pelvic pain and where is pelvic pain located?
Pelvic pain is any pain that occurs in the region of the lower abdomen, reproductive organs, pelvic floor or sacrum. The pain can be a dull ache or a stabbing pelvic pain. Pelvic pain can arise as a result of one or more conditions and can impact both men and women, though it is generally more common in women. Pelvic pain can present differently in everyone depending on the cause of pain, but it is always important to see a healthcare professional, starting with your medical doctor or OB/GYN if you have pelvic pain. If your pain is severe, comes on suddenly, you have never had pelvic pain before, or if it is accompanied by any of the symptoms below, go to the emergency room as soon as possible:
- Pain or bleeding when you pee or poo
- Pain during sex
- Fever or chills
- Pain in the groin or hip area
- Diarrhea or constipation
- Intense bloating or gas
- Vaginal bleeding, spotting or discharge which is abnormal for you
- Abnormal menstrual pain (anything beyond the usual cramps that may accompany your period)
Your medical doctor will take a history from you, usually examine the painful area and refer you for imaging or lab tests as needed. It is important to see a doctor right away so that they can determine the cause of your pain and refer you for the appropriate treatment as soon as possible. In many cases of pelvic pain, early detection and treatment of the cause leads to better health outcomes.
What causes pelvic pain?
| Possible causes of pelvic pain in both men and women | Possible causes of pelvic pain in people designated female at birth |
| · Appendicitis · Sexually transmitted infection · Urinary tract infections/bladder infection · Kidney infection/stones · Hernia · Intestinal conditions (diverticulitis, Crohn’s disease, IBS, intestinal obstruction) · Pelvic disorders (spasms of pelvic muscles) · Direct injury (fall on tailbone or pubic bone or direct blow to the pelvic floor) or pelvic fracture · Nerve conditions (pinched nerves in the spine or pelvic area) · Psychogenic pain (from past trauma, abuse or stress) · Colon cancer · Fibromyalgia Pelvic organ prolapse |
· Menstrual cramps · Pregnancy or ectopic pregnancy · Miscarriage · Ovulation · Endometriosis · Uterine fibroids · Ovarian cysts or ovarian disorders · Pelvic inflammatory disease · Cervical, uterine or ovarian cancer *People designated male at birth may also experience pelvic pain related to prostatitis or prostate cancer. *Note that this list is not exhaustive of the causes of pelvic pain. The best way to know the cause of your pelvic pain is to see your medical doctor. |
If the cause of your pelvic pain is related to the musculoskeletal system, sometimes you may be referred to a physical therapist, chiropractor, massage therapist, acupuncturist or other healthcare provider for treatment.
Pelvic floor dysfunction
Pelvic floor dysfunction is a common condition where sufferers have trouble correctly coordinating the movement of muscles in their pelvic floor. This means that they may have trouble properly urinating or defecating, may feel pain during sex or, if they have a penis, they may struggle with erectile dysfunction. Pelvic floor dysfunction symptoms can include:
- feeling like you need to use the bathroom all the time
- starting and stopping many times during urination or bowel movements
- frequent constipation or feeling like you need to strain or push hard to have a bowel movement
- pain during defecation or urination
- fecal or urinary incontinence or leaking
- low back pain without any other cause or ongoing pelvic, rectal or genital pain
Pelvic floor dysfunction can occur with pregnancy, advancing age, being overweight, pelvic surgery, traumatic injury to the pelvis or even with pelvic muscle overuse.
If you are experiencing the symptoms noted above, see a medical doctor as soon as possible. Many patients with pelvic floor dysfunction are referred for specialized pelvic physiotherapy and in some cases may be referred for counselling if there are underlying psychological factors contributing to the dysfunction.
Pelvic pain in pregnancy
If you have pelvic pain during pregnancy, you aren’t alone. Pelvic girdle pain (PGP) is relatively common and ranges from mild discomfort to a severe disability in pregnant people. Generally PGP can cause pain, instability, limited mobility and reduced functioning in any of the three pelvic joints (pubic joint, sacroiliac joints).
PGP can begin as early as the first trimester of pregnancy and usually starts as pain low in the abdomen over the pubic bone. Pain from PGP can also be noticeable in the hips, gluteal region or groin and may radiate down the thighs, usually on the inner side. PGP pain may remain mild or could gradually worsen in severity as the pregnancy progresses.
PGP can cause a pregnant person to waddle or shuffle and they may start to hear clicking or popping sounds coming from their pelvic region. People with PGP may also have pain when they walk, go up and down stairs or turn over in bed.
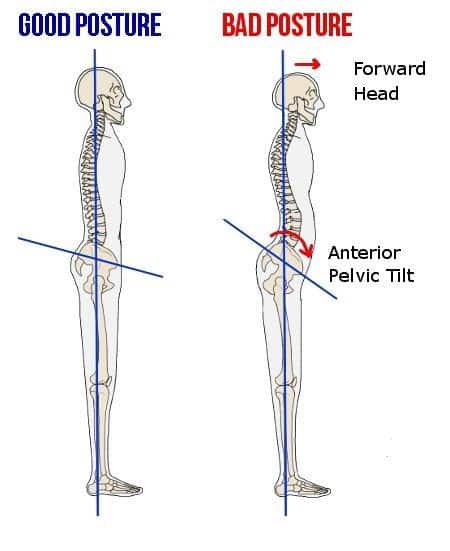
PGP usually arises because of a combination of:
- pregnancy related postural changes
- changes in the centre of gravity for the pregnant person
- the weight of the baby against the pelvis
- unstable pelvic joints
- the influence of pregnancy hormones on pelvic ligaments and tendons
PGP can occur suddenly due to a fall, a strain on the pelvic joints, or a sudden slip that forces the legs apart too quickly.
If you’re pregnant and experiencing pelvic pain, your first step should be a visit to your doctor. They will check your pregnancy’s progress and rule out other causes of pain. If needed, they may refer you to a chiropractor, physiotherapist, or another healthcare provider for treatment and pain management.
These specialists will address joint, ligament, and muscle issues, provide education, and recommend rehab exercises. They may also suggest assistive devices like trochanteric belts, braces, girdles, or specialized taping to improve comfort during pregnancy.
In many cases, pelvic girdle pain resolves after delivery. However, some women may need extended postpartum treatment if the pain persists.
Pelvic pain in women
Pelvic pain tends to be more common in women (or those assigned female at birth) due to a variety of factors unique to female physiology and anatomy. One of the most common reasons for pelvic pain in those with female anatomy is menstruation-related cramping or dysmenorrhea. Cramping can range from mild to very severe or even crippling in some people. There are a variety of at home and clinical treatment options for cramps which can include:
- Using heat
- Using a TENS machine
- Reducing stress and exercising regularly
- Improving your diet or using supplements like vitamin E, vitamin B6, vitamin B1, magnesium or Omega-3 fatty acids
- Pain relievers –over the counter or prescribed
- Acupuncture or acupressure treatments
- Hormonal birth control
- Surgery – if your cramps are related to endometriosis or fibroids
In any case of pelvic pain, it is important to see your medical doctor or OB/GYN to have them properly diagnose the cause of your pain.
Pelvic bone pain
If you have pelvic bone pain, it may come from the sacroiliac joints, the pubic joint, or an underlying condition like metastatic cancer, infection, Paget’s disease, osteoporosis, or an undiagnosed fracture. To find the cause, start by booking an appointment with your doctor. They will take your medical history, perform an exam, and order necessary tests such as X-rays, CT scans, or MRIs.
Pelvic Floor Exercises
Pelvic tilt
- Lay on your back with your arms across your chest and bend your knees to put your feet flat on the floor
- Make your hips rotate by pushing your low back into the floor then rotate your hips the other way slightly lifting your low back off the floor.
Knee to chest stretch
- Lay on your back and pull one knee toward your shoulder with your hands
- Hold 30-60 seconds on each side
Bridge with toes up
- Lay on your back with your arms across your chest
- Raise your knees so your feet are placed flat on the floor
- Pull your toes off the floor and rock back onto your heels
- Slowly raise your buttocks off the ground as high as you can into bridge position
- Lower back to the ground and repeat 10-20 times.
Seated march with band
- Sit in a chair and put a theraband around your thighs (so it sits above your knee)
- Pick one leg up against the resistance of the band as if you are marching and then lower it. Repeat with the other leg.
- Perform 10-20 repetitions on each leg
Crunch
- Lay on your back with your knees bent and your arms beside you or behind your head to support it
- Keep your head relaxed and crunch your abdominal muscles to lift your shoulders off the floor slightly.
*A note on care for pelvic pain: the pelvis is a sensitive area for many people and you may not be comfortable having these areas examined or treated. Sometimes these exams or treatments are necessary, but be aware that your healthcare provider should always explain in advance where they need to examine (observe or touch) and the purpose of any exam or treatment. They should also get your express consent before they perform any examination or treatment. You also have the right to have another individual present for any examination or treatment including a support person or another healthcare[h1] professional. If at any time you feel uncomfortable with a pelvic exam or treatment you have the right to withdraw consent and stop the procedure. Healthcare professionals have a duty to act ethically and ensure patients are treated safely and in a manner that respects patient’s boundaries, comfort and dignity.
We at the Unpain clinic in Edmonton, hope that you have found this information helpful and informative. If you have any questions about pelvic pain, feel free to book a no obligation telehealth consultation with our physiotherapist or chiropractor. Even if we can’t treat your pain, we are happy to point you in the direction of the healthcare professional who can.
FAQs about Pelvic Pain
What are pelvic pain symptoms?
Pelvic pain is pain that occurs in the pelvic floor, lower abdomen, sacral, groin or genital region. This pain may be accompanied by pain or bleeding when you pee or poo, pain during sex, pain in the hip region, fever or chills, diarrhea or constipation, intense gas or bloating, abnormal vaginal bleeding, spotting or discharge or abnormal menstrual pain (anything beyond the usual cramps).
Pelvic pain when walking – what is going on?
While there can be some exceptions, pelvic pain when walking is often related to an issue with your musculoskeletal (MSK) system (bones, joints, ligaments, tendons and muscles). The most common causes of pelvic MSK pain include: Sacroiliac joint pain, osteitis pubis, pubic joint dysfunction, pelvic floor muscle pain or inguinal hernia.
Should I see a physiotherapist if I have pelvic pain?
Yes, depending on the cause of your pelvic pain, but it is important to make sure you see a medical doctor to have them rule out non-musculoskeletal causes of pain first (e.g. cancer, infections, organ disease or dysfunction). There are even physiotherapists who have extra training in working with patients who suffer from pelvic pain. You do not need a referral from your medical doctor to see a pelvic physiotherapist.
Is physio or chiropractic safe for pregnancy related pelvic pain?
As long as your pregnancy is healthy and progressing normally, physio and chiropractic can be safe during pregnancy. There is no evidence of harm to the pregnant person or fetus when treatments are applied safely and appropriately, however some practitioners may not be comfortable treating women in their first trimester or before 20 weeks gestation due to the high natural rate of miscarriage (10-15% or greater).
I have pelvic pain when lying down at night – what’s happening?
Your nighttime pain could be a sign that your sleeping position may be irritating your joints. Additionally, your buttock muscles are not active when in a resting position which means the pelvic bones are not being stabilized in the same way as when you are awake. Some people may also experience more muscle spasms in the pelvic floor at night than during the day.
If you are having more pain at night, especially if the pain escalates far beyond what you experience during the day, it is important that you see your medical doctor for an exam as soon as possible.
How do you relieve pelvic pain when sleeping?
Try putting a pillow between your knees when lying on your side. The pillow will help align your pelvis and may help relieve pressure on the joints and soft-tissues.
True Shockwave™ or Flashwave®? No need to wonder.
Our therapists will assess your situation and formulate a True Shockwave™, Radial Pressure Wave or Flashwave® treatment plan appropriate for achieving the most effective and lasting results.